Male breast cancer patient denied Medicaid because of his gender
Last month, 26-year-old Raymond Johnson discovered he was one of the estimated 2,100 men who are diagnosed with breast cancer each year. But despite the reality that breast cancer in men is a well-established medical fact, Medicaid, a health insurance program for low-income and disabled Americans, denies coverage to a number of male breast cancer victims.
Johnson, a trader making $9/hour, worked for a small organization that does not provide health insurance. Because of the recession, he was working only 30 hours per week and could not afford private insurance.
After seeking medical attention for chest pains at his local emergency room, Johnson was diagnosed with breast cancer. “I didn’t even know men could get breast cancer,” Johnson said. “I’m young. I didn’t think anything bad could really happen to me.”
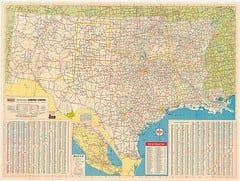
Since the single South Carolina man did not meet the qualifications for traditional Medicaid, he was urged by the hospital where he was receiving treatment to seek help under The Breast and Cervical Cancer Prevention and Treatment Act.
The Breast and Cervical Cancer Prevention and Treatment Act is an 11-year-old federal law that utilizes funds from Medicaid to aid breast or cervical cancer patients who are denied by Medicaid because their income is too high, Jeff Stensland, spokesperson for the South Carolina Department of Health and Human Services explains.
Although the eligibility rules for coverage under the Act are complex, Johnson met all, except for one: Johnson is not a woman. “We want to cover this guy,” Stensland says, “but we simply can’t.”
Even though today, Johnson described himself as feeling “pretty good,” he is still undergoing chemotherapy and his treatment may require surgery to treat his Stage II cancer. His main concern now is how he is going to pay for his care.
The South Carolina Department of Health and Human Services has tried more than once to get coverage under The Breast and Cervical Cancer Prevention and Treatment Act for male patients. There were two other men in the last four years who met all other aspects of the act’s criteria, but have been denied coverage under the act simply because they are men. “We’re in conversations with the federal government on this issue,” Stensland says. “It’s clearly discriminatory, and we believe it’s a good example of an overly rigid interpretation of the law, a law that’s designed to help patients with these cancers.”
“I just can’t tell you how floored I was when I got that letter saying I didn’t quality for help,” Johnson says. “The bills are going to be huge. I have breast cancer. I really don’t see how that’s possible.”
In an email, a spokesperson from the Center for Medicare and Medicaid tells msnbc.com: “The law governing this specific program is linked to a CDC screening program. We are working with the CDC and South Carolina to see what options may exist to address this situation. We are committed to ensuring that all individuals who would be eligible for this program have coverage.”
Read more about this here.